Introduction
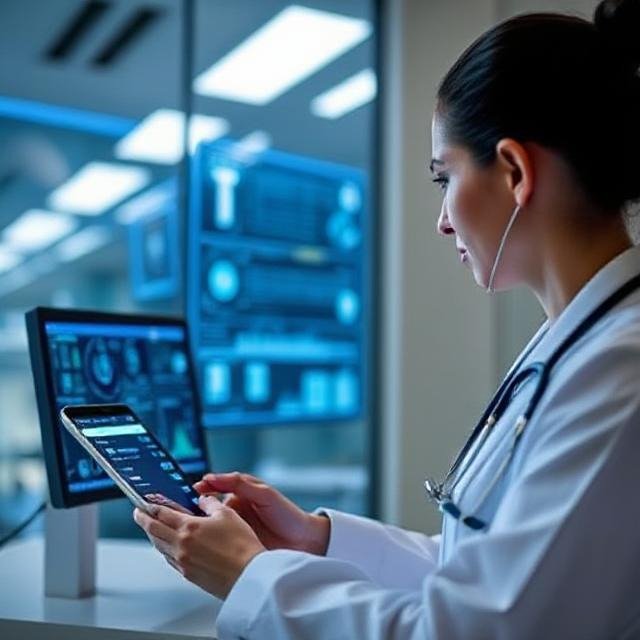
The healthcare industry is undergoing a monumental transformation. At the heart of this shift lies the concept of the SMART hospital—a technologically advanced ecosystem where digital tools streamline operations, enhance clinical care, and elevate patient experiences. Among the foundational technologies powering these futuristic hospitals, telemedicine and remote patient monitoring (RPM) stand out as the backbone.
Not only do these tools empower patients with real-time access to medical care from anywhere in the world, but they also reshape how hospitals function—making them more responsive, efficient, and sustainable. As healthcare providers aim to evolve into green hospitals, the integration of telehealth and remote monitoring technologies becomes essential for energy savings, space optimization, and environmentally responsible healthcare delivery.
This blog explores how telemedicine and remote monitoring are pivotal to the smart hospital model, how they contribute to sustainable growth, and why every hospital planning blueprint today must consider them as foundational pillars.
1. Understanding Telemedicine and Remote Monitoring
What is Telemedicine?
Telemedicine involves the remote diagnosis, consultation, and treatment of patients using telecommunications technology. It allows patients to connect with physicians, specialists, and healthcare providers through:
-
Video conferencing
-
Mobile apps
-
Online portals
-
Wearables and IoT devices
What is Remote Patient Monitoring (RPM)?
RPM is a subset of telehealth that uses connected digital tools to record, transmit, and analyze health data in real-time. These may include:
-
Blood pressure monitors
-
Glucose monitors
-
ECGs
-
Sleep trackers
-
Pulse oximeters
By combining these with cloud platforms and AI analytics, healthcare providers can monitor chronic conditions, prevent emergencies, and deliver timely care without requiring the patient to be in a hospital bed.
2. The Role of Telemedicine in SMART Hospitals
In the smart hospital environment, telemedicine isn’t just a convenience—it’s a necessity.
Enhancing Accessibility
Telemedicine allows hospitals to deliver care to remote areas, underserved populations, and immobile patients. This bridges the urban-rural divide and reduces geographical disparities in healthcare access.
Improving Efficiency
Virtual consultations help reduce the burden on emergency departments and OPDs. Non-critical patients can get timely advice without overwhelming in-hospital resources.
Cost Reduction
-
Less infrastructure needed for outpatient visits
-
Fewer patient no-shows
-
Lower transportation and logistics costs
These savings directly contribute to the financial sustainability of green hospital models.
Integration with AI and EHRs
AI chatbots and virtual assistants can pre-screen patients, update Electronic Health Records (EHRs), and guide them through scheduling, prescriptions, and follow-ups—freeing up clinical staff for more complex cases.
3. Remote Monitoring: From Reactive to Proactive Healthcare
Real-Time Data = Real-Time Decisions
RPM tools feed live health metrics into hospital dashboards, enabling healthcare providers to:
-
Detect deteriorating conditions early
-
Adjust medication dosages remotely
-
Intervene before a minor issue escalates
This proactive approach can prevent unnecessary hospitalizations and ICU admissions.
Chronic Disease Management
Patients with diabetes, hypertension, COPD, and heart failure benefit greatly from RPM. Doctors can personalize treatment plans based on trends, not just snapshots from hospital visits.
Elderly and Post-Operative Care
RPM helps older adults remain independent while still being monitored. Post-surgery patients can heal at home under virtual observation, reducing hospital stays and infection risks.
4. The Environmental Impact: A Boost for Green Hospitals
Telemedicine and remote monitoring are more than digital solutions—they are green solutions.
Reduced Carbon Footprint
-
Fewer physical visits mean less travel-related emissions
-
Lower demand for on-site energy, water, and waste services
-
Reduced paper usage due to digital records and prescriptions
Space Optimization
Less need for physical infrastructure—like waiting rooms and outpatient blocks—frees up resources and allows for smarter, greener hospital planning.
Sustainable Workforce Management
Virtual care enables flexible work models for healthcare professionals, reducing commuting and enabling round-the-clock care with lower operational energy costs.
5. Telehealth Infrastructure in Hospital Planning
Every new healthcare facility being designed today must include telehealth integration from the ground up.
Smart Hospital Architecture Considerations
-
Dedicated teleconsultation rooms with soundproofing and ergonomic lighting
-
High-speed, secure internet infrastructure
-
IoT-compatible patient rooms
-
Modular spaces that can be reconfigured for hybrid (in-person + virtual) care
Tech Stack Essentials
-
Interoperable EHRs
-
Video conferencing APIs
-
Cloud storage with advanced cybersecurity
-
Data analytics platforms for predictive insights
Staff Training and Change Management
No telehealth plan is complete without training clinicians and support staff in digital tools and workflows. A smart hospital is only as effective as its users are adaptable.
6. Economic and Operational Benefits
Cost-Effectiveness
-
Fewer admissions and shorter stays lead to direct cost savings
-
Improved resource allocation through predictive patient volume analytics
-
Reduced need for hospital readmissions with continuous virtual follow-up
Revenue Opportunities
-
Subscription-based remote monitoring services
-
International teleconsultations
-
Insurance reimbursement for virtual visits (increasingly common)
Resilience in Crisis Situations
The COVID-19 pandemic demonstrated the critical role of telemedicine in maintaining continuity of care. A smart hospital with remote infrastructure is better equipped to handle:
-
Pandemics
-
Natural disasters
-
Staff shortages
-
Systemic disruptions
7. Patient Experience in the SMART Hospital Era
Patient satisfaction is increasingly tied to convenience, personalization, and digital empowerment—all of which telemedicine and RPM deliver.
Benefits for Patients
-
Access to care from home
-
Shorter wait times
-
Continuous monitoring without hospital admission
-
Educational tools and health literacy apps
Empowerment Through Data
Patients can view their health metrics, get alerts, and take informed actions—making healthcare a collaborative process rather than a one-way interaction.
8. Global Case Studies: Leading the Telehealth Revolution
Cleveland Clinic (USA)
Uses remote monitoring for heart failure and post-operative care, reducing readmissions by over 25%.
Narayana Health (India)
Delivers tele-ICU services to rural hospitals, enhancing care without needing to transfer critical patients.
Sheba Medical Center (Israel)
Has developed a fully virtual hospital wing during the pandemic, showcasing how a smart hospital can rapidly adapt using telemedicine.
9. Challenges and Considerations
While the benefits of telemedicine and remote monitoring are profound, the road to full-scale implementation within a smart hospital framework is not without obstacles. To truly realize the potential of these technologies, we must address a range of challenges that span privacy, equity, regulation, and infrastructure.
1. Data Privacy and Compliance
The collection, transmission, and storage of patient data through telemedicine platforms and remote monitoring devices pose serious concerns around privacy and security.
-
Healthcare providers must comply with stringent data protection laws such as HIPAA (Health Insurance Portability and Accountability Act) in the U.S. and GDPR (General Data Protection Regulation) in the EU.
-
Any breach in data security can erode patient trust and result in severe financial penalties.
-
Encryption, multi-factor authentication, secure cloud services, and robust cybersecurity protocols must become standard in smart hospital digital architecture.
-
As part of future-ready hospital planning, cyber-resilience strategies need to be integrated from the ground up.
2. Bridging the Digital Divide
While telehealth promises to expand access to care, it also risks widening health disparities if not implemented inclusively.
-
In rural, tribal, or economically disadvantaged areas, poor internet connectivity, lack of digital literacy, and insufficient access to smart devices can hinder adoption.
-
Senior citizens, persons with disabilities, and non-English speakers may find it challenging to navigate telemedicine platforms.
-
Equitable access must be a core design principle in the smart hospital framework, including provisions for telehealth kiosks, mobile clinics, and community outreach programs.
-
Government initiatives and public-private partnerships are needed to ensure that digital health doesn’t leave vulnerable populations behind.
3. Evolving Reimbursement and Regulatory Frameworks
One of the biggest bottlenecks for telemedicine growth has been the lack of clarity and consistency in reimbursement models and licensing regulations.
-
Many healthcare systems are still catching up to define how virtual consultations and remote monitoring should be billed.
-
In cross-border or interstate telehealth, there may be legal limitations on where and how physicians can practice.
-
Insurance providers, both public and private, must establish permanent and fair reimbursement structures to incentivize providers.
-
Regulatory bodies need to modernize policies to accommodate AI-driven consultations, wearable diagnostics, and decentralized care—key pillars of the smart hospital concept.
4. Technology Adoption Among Older Adults and Non-Tech Users
Although remote care is ideal for managing chronic diseases and providing post-operative support to elderly patients, adoption remains slow among these groups.
-
Cognitive barriers, technophobia, or physical limitations (vision, dexterity, hearing) can make it difficult to use telehealth tools independently.
-
Smart interfaces, voice-enabled technologies, caregiver training, and support hotlines are essential for inclusive digital care.
-
Designing devices and platforms with user-centric thinking—especially for aging populations—should be a key focus in telemedicine development.
5. Integration with Existing Health Systems
Another major challenge is ensuring seamless integration of telemedicine and RPM platforms with existing hospital infrastructure and Electronic Health Records (EHRs).
-
Many hospitals operate on legacy systems that are not interoperable with modern IoT devices or third-party telehealth platforms.
-
Without a cohesive data ecosystem, care coordination suffers, and digital tools become siloed and underutilized.
-
During the hospital planning phase, IT architecture must be designed to support plug-and-play capabilities, scalable APIs, and centralized data repositories.
6. Clinical and Ethical Considerations
Not every condition can be treated remotely. Telehealth should complement, not replace, hands-on clinical evaluations.
-
There’s a risk of over-reliance on virtual care for conditions that require physical examination, lab diagnostics, or surgical interventions.
-
Ethical dilemmas may arise when making critical decisions based on limited remote data, especially in emergencies.
-
Developing clear protocols on when to escalate care from remote to in-person is crucial for safe and responsible digital healthcare delivery.
7. Environmental Trade-Offs
While telemedicine contributes to green hospital goals by reducing emissions and conserving energy, the surge in digital infrastructure brings its own environmental footprint.
-
Data centers, smart devices, and electronic waste from obsolete hardware can offset some of the environmental gains.
-
Responsible hospital planning should include energy-efficient data storage, e-waste recycling, and the use of low-emission telehealth hardware.
In conclusion, the transition to a telehealth-powered smart hospital is a complex journey—one that requires thoughtful planning, inclusive design, and continuous innovation. Technology alone cannot solve healthcare’s greatest challenges. Instead, smart solutions must be paired with smart policies, ethical practices, and human-centered design to ensure that virtual care is equitable, secure, and sustainable.
By addressing these challenges proactively, healthcare institutions can build future-ready hospitals that are not only technologically advanced but also environmentally responsible and socially inclusive.
10. The Road Ahead: Telehealth and RPM in Future SMART Hospitals
AI-Powered Teleconsultations
AI will assist doctors during virtual consultations, providing decision support, diagnostics, and even language translation in real-time.
Augmented Reality and Virtual Reality
Remote procedures, immersive rehabilitation, and virtual rounds using AR/VR are set to redefine patient and doctor experiences.
Integration with Wearables and Home Assistants
Telemedicine will be embedded in daily life through smartwatches, voice assistants, and home diagnostic kits—extending the hospital into the home.
Smart Public Health Monitoring
Telehealth data can be aggregated and anonymized to track public health trends and predict outbreaks—turning hospitals into community health command centers.
Conclusion
Telemedicine and remote monitoring are no longer optional—they are foundational to the smart hospital vision. These technologies redefine how hospitals operate, how patients engage, and how care is delivered in the 21st century.
Beyond convenience and cost-effectiveness, they support environmental stewardship—making them a cornerstone of green hospital development. And when considered in hospital planning from day one, they unlock new possibilities for scalable, resilient, and sustainable healthcare infrastructure.
The backbone of tomorrow’s hospitals won’t be built solely from steel and concrete. It will be woven with data, powered by connectivity, and driven by human empathy enhanced through intelligent automation. The smart hospital is here—and telehealth is its pulse.